A novel remedy primarily based on induced neuronal stem cells shows promise in a mouse model of Alzheimer’s disease – and it may be administered intranasally [1].
Who wants cells?
Stem cell therapies have made nice strides in latest many years. They’ve been efficiently employed towards quite a few ailments, from most cancers to osteoarthritis. Nevertheless, storing, transporting, and administering cells isn’t straightforward. Furthermore, in some instances, cells, with their terribly complicated metabolisms, can produce undesirable unwanted effects. As an illustration, neural stem/progenitor cells (NSCs) have been proven to enhance signs of sure mind ailments [2] however can even set off pathological modifications within the mind [3].
Nevertheless, the entire cell may not at all times be essential. Cells have been identified to speak with one another by excreting extracellular vesicles (EVs), tiny membrane-bound bubbles that may carry varied cargoes, corresponding to RNA molecules and proteins. Scientists have discovered to reap vesicles produced by cells and administer them domestically or systemically, typically recapitulating a lot of the impact of cell administration.
Not like stem cells, EVs could be frozen and thawed with out compromising their therapeutic efficacy. Moreover, cells of various varieties can now be simply produced from induced pluripotent stem cells (iPSCs). These are somatic cells reverted into pluripotency by making use of sure molecules, corresponding to the unique reprogramming cocktail of Yamanaka components (OSKM).
Much less irritation
In a brand new research revealed within the Journal of Extracellular Vesicles, researchers from Texas A&M College took human iPSCs and re-differentiated them into NSCs. They then harvested the extracellular vesicles produced by the cells, purified them, and administered them intranasally to a mouse mannequin of familial Alzheimer’s illness (5xFAD mice). Regardless of many years of analysis and tens of billions of {dollars} spent, a remedy for Alzheimer’s stays elusive.
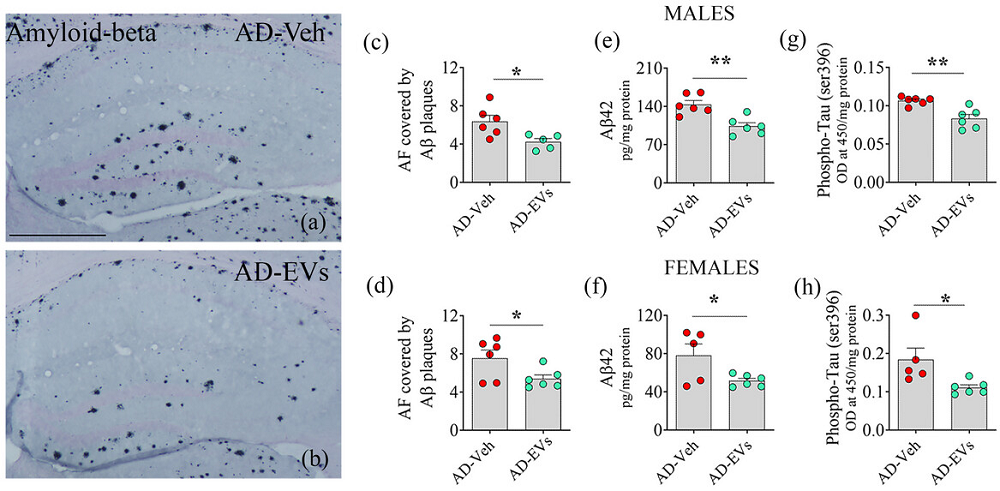
Whereas mouse fashions of Alzheimer’s have their limitations, as mice naturally don’t develop this illness, 5xFAD mice have been extensively used. These animals begin displaying Alzheimer’s-like pathologies, corresponding to amyloid beta (Aβ) plaques and elevated neuroinflammation on the age of three months, which is when the therapy was administered. About two months later, the mice underwent cognitive and neuropathological assessments.
The researchers confirmed that the EVs had been certainly taken up by the mind’s resident macrophages (microglia). In Alzheimer’s, these cells encompass Aβ plaques, presumably in an try to take away them. They show elevated activation and irritation, which has been linked to illness development.
“Extended activation causes microglia to lose their regular operate and start to hurt neurons, resulting in progressive neuron loss,” explains Ashok Okay. Shetty, Ph.D., a College Distinguished Professor and affiliate director on the Institute for Regenerative Drugs within the Division of Cell Biology and Genetics, and the corresponding creator on the research.
RNA sequencing revealed that the therapy downregulated a number of inflammation-related pathways that had been considerably upregulated in 5xFAD mice in comparison with wholesome controls. Notably, this occurred with out compromising the microglia’s phagocytosis operate: their potential to engulf and destroy pathogens.
The therapy additionally led to a major discount within the burden of Aβ plaques and phosphorylated tau protein, two main hallmarks of Alzheimer’s. Whereas each sexes confirmed enhancements, males demonstrated a extra sturdy response to the therapy.
By the age of 5 months, 5xFAD mice sometimes exhibit important cognitive decline, which was additionally noticed on this research. The EV therapy, nonetheless, appeared to successfully block this decline. Checks included the article location take a look at, through which cognitively wholesome animals are anticipated to spend extra time exploring an object in a novel place than in a well-recognized place, and the sample recognition take a look at, which measures the power to discern novel objects from acquainted ones.
Curiously, the researchers additionally assessed the mice’s temper. Temper modifications are more and more gaining recognition as a clinically vital side of Alzheimer’s illness. Identical to many human Alzheimer’s sufferers, untreated 5xFAD mice exhibited anhedonia, the lack to get pleasure from issues – on this case, sweetened water. The EV therapy restored the rodents’ joie de vivre – or at the very least their choice for sugar.
Related results in human cells
Whereas the researchers didn’t take a look at their therapy in human sufferers, they pursued the following greatest different: making use of NSC-derived EVs to human microglia in vitro. When challenged with Aβ-42, an isoform of Aβ identified for its excessive aggregation propensity and central position within the pathology of Alzheimer’s illness, microglia exhibited overactivation and an inflammatory phenotype. These results, nonetheless, had been reversed by the EV therapy.
In keeping with the paper, EVs are superior to NSCs in that they don’t replicate and readily cross the blood-brain barrier. Intranasal administration is straightforward, non-invasive, and characterised by fast motion. Whereas the research was performed on animals at early levels of the illness, fixed advances in diagnostics make this much less of a limitation.
“This method is efficient as a result of the cargo carried by these extracellular vesicles might scale back the neuropathological modifications within the mind,” says Shetty, who has filed a patent on the intranasal software of neural stem cell-derived extracellular vesicles for treating Alzheimer’s and different neurological problems. “Our journey to advance the applying of this remedy for Alzheimer’s illness is simply starting.”
Literature
[1] Madhu, L. N., Kodali, M., Upadhya, R., Rao, S., Somayaji, Y., Attaluri, S., … & Shetty, A. Okay. (2024). Extracellular vesicles from human‐induced pluripotent stem cell‐derived neural stem cells alleviate proinflammatory cascades inside illness‐related microglia in Alzheimer’s illness. Journal of Extracellular Vesicles, 13(11), e12519.
[2] Temple, S. (2023). Advancing cell remedy for neurodegenerative ailments. Cell stem cell, 30(5), 512-529.
[3] Abdi, S., Javanmehr, N., Ghasemi-Kasman, M., Bali, H. Y., & Pirzadeh, M. (2022). Stem cell-based therapeutic and diagnostic approaches in Alzheimer’s illness. Present Neuropharmacology, 20(6), 1093-1115.






